Care & services offered at the CDMD dental center
PERIODONTICS
Extensive assessment procedures
The foundations of natural, restored or implanted teeth are healthy gums and bones. Statistics tell us that 90% of adults have gum disease of varying degrees of severity at some point in their lives, and that three-quarters of adults over the age of 50 suffer from a disease called periodontitis, c ie damage to the superficial and deep periodontal tissues with loss of attachment and inflammation of the gums. Periodontitis or periodontal disease can be localized to a single tooth or generalized. The more periodontitis progresses, the more bone is lost, with periods of remission and exacerbation, which can lead to the loss of the tooth itself. Recent research shows that periodontitis has links with various diabetes,
Our goal is to quickly diagnose this disease so that you can reduce its progression and related bone loss so that you can keep your smile for a long time. In any case, daily care at home and the annual consultation of his doctor play an essential role in the prevention program that follows .
What are the causes of periodontitis?
The plaque
 Plaque is the main cause of periodontal disease. Every day, a small invisible and sticky film is deposited on the teeth. This film is the plaque, in which colonies of bacteria live and multiply. There are also some food fragments and saliva in the plaque. When there are many of them, the plaque is seen especially at the edge of the gums; it calcifies to form tartar if it remains stuck to the teeth.
Plaque is the main cause of periodontal disease. Every day, a small invisible and sticky film is deposited on the teeth. This film is the plaque, in which colonies of bacteria live and multiply. There are also some food fragments and saliva in the plaque. When there are many of them, the plaque is seen especially at the edge of the gums; it calcifies to form tartar if it remains stuck to the teeth.
Plaque bacteria produce toxins that inflame the gums, and this inflammation signals the onset of periodontitis. If the inflammation is not controlled, the progressive destruction of bone sets in, without the manifestation of symptoms at the beginning of the disease. When a significant part of the bone has been lost, the tooth begins to be unstable, most of the time without realizing it (since there is no pain). As soon as a tooth loosens, the destruction of the surrounding bone accelerates, especially if there is also an occlusion problem. Finally, deprived of much of the supporting bone, the tooth becomes so unstable that it falls out or has to be removed.
Nutrition
Our body is partly dependent on what we eat. Good, whole foods and a healthy lifestyle help maintain a healthy body.
The stress
Negative stress is also a factor in the emergence of the disease. For example, a person’s resistance, which has been normal for years, can suddenly decrease for no apparent reason. Then, periodontitis appears or there is a resurgence of periodontitis that had been controlled. It is difficult to find why resistance varies from person to person, and why it varies from moment to moment in the same person. Dentistry research teams around the world are looking into this question. How can we manage our resistance and our immune response?
Cigarette
Tobacco poses a significant risk of developing severe periodontitis. Those who belong to the category of moderate smokers, that is to say ten or more cigarettes a day, and those who belong to the category of heavy smokers are more likely than others to develop severe periodontitis (respectively two and seven times more). Tobacco use also results in more frequent resurgence of disease and waning response to treatment. It is generally believed that this is due to the fact that, in smokers, more bacteria accumulate under the gum line than in non-smokers, and that there is a deficiency of vitamin C. Following surgical treatment or non-surgical, healing in these cases may be delayed.
In addition, the use of tobacco has the effect of reducing tissue inflammation and bleeding, even during the introduction of the probe. In these cases, periodontal pockets and severe bone loss are likely overlooked. Smokers are more at risk than non-smokers of developing other diseases repeatedly. In this regard, they must be closely monitored and receive, four times a year, hygiene care that will help them meet the challenge of eliminating these bacteria.
How to assess and diagnose periodontitis?
- Examination and visual appearance (redness and swelling): Uses magnifying glasses that magnify the area observed 4.5 times; at the complete examination, each tooth is scrutinized. Halogen lighting eliminates all possible shadows.
- Measurement of the depth of the pockets : that of 3 mm denotes a normal situation; that of 4 mm and more indicates the presence of disease, in most cases.
- Bleeding and swelling : means that there is inflammation.
- Instability: may be related to bone loss.
- Bone loss up to the furcation : that is, bone lost between the roots of the molars or between those of the upper first premolars.
- Recession – exposed root surface : can mean lost bone or too vigorous tooth brushing.
- Constant bad breath : could be a sign of periodontitis.
- Bone loss : can be picked up by scanned x-rays.
How to prevent them?
- Brush your teeth properly (at least three times a day after meals) and floss (at least once a day) to remove all plaque.
- Have your gums and periodontium examined regularly by the dentist.
- Complete the recommended treatments.
- Manage stress.
- Eat healthy, whole foods.
- Quit smoking if possible.
Diagnosis of periodontitis
- Health
- Active gingivitis
- Periodontal pockets less than 4 mm with bleeding
- Onset of periodontitis
- Onset of bone loss
- Periodontal pockets of 4 to 6 mm (with bleeding)
- Furcation: severity level I
 This film shows bone loss with increased pocketing and buildup of tartar, or calculus, on teeth below gum level, where it is difficult to see.
This film shows bone loss with increased pocketing and buildup of tartar, or calculus, on teeth below gum level, where it is difficult to see. - Average periodontitis
- 30-50% bone loss
- 5 to 8 mm periodontal pockets
- Furcation: severity level I and II
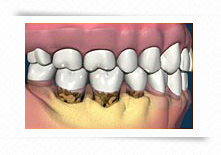 This film shows bone loss with increased pocketing and buildup of tartar, or calculus, on teeth below gum level, where it is difficult to see.
This film shows bone loss with increased pocketing and buildup of tartar, or calculus, on teeth below gum level, where it is difficult to see. - Advanced periodontitis
- Bone loss of more than 50%
- Periodontal pockets larger than 8 mm
- Furcation: severity level II and III
 This film shows bone loss with increased pocketing and buildup of tartar, or calculus, on teeth below gum level, where it is difficult to see.
This film shows bone loss with increased pocketing and buildup of tartar, or calculus, on teeth below gum level, where it is difficult to see.
Recommendations and treatments
| Cleaning and preventive examination: 6 months to 12 months, depending on risk factors | Antibacterial mouthwash |
| Manual toothbrush | Electric toothbrush |
| Irrigation | Management without surgery |
| Periodontal hygiene instruments | Scaling and curettage |
| Nutritional supplements | Local application of drugs |
| Surgical treatment | Regeneration |
| Taking antibiotics | Restorations to stabilize |
| Extractions | Cleaning every 2, 3, 4 or 6 months |
